Abstract
Introduction
Primary immune thrombocytopenia is an autoimmune disorder characterized by low platelet counts due to increased destruction and insuficient production, with various propensity for bleeding. Corticosteroids are first choice of treatment for newly diagnosed ITP. There is a controversy about a choice of "better" corticosteroid between prednisone and dexamethasone. Although in different studies high dose dexamethasone did not show a clear benefit considering the long term sustained response, it is confirmed that it raises platelet levels faster, with possible fewer side effects compared to prednisone. Guidelines suggest shorter treatment with corticosteroids and early use of second line treatment, usually TPO RAs. Also, in the age of COVID, avoiding prolonged treatment with steroids could be beneficial.
Methods
In this retrospective study we analyzed newly diagnosed ITP patients treated with high dose dexamethasone (HD-DXM) from 1.1.2018 to 31.12.2021. Patients received 40 mg of dexamethasone once daily for 4 consecutive days. Following data was extracted from electronic patients' records: age, gender, date of diagnosis, initial platelet count, date of treatment, platelet count at a start of treatment and on days 7 and 14, at 3 months, 6 months, 12 months and 24 months and date of relapse. Due to the retrospective nature of data collection, we allowed deviation of 3 days for the day 7 and day 14 platelet counts and up to 3 weeks for the other dates. Complete response (CR) was defined as a platelet count ≥100 x 109/L. Response (R) was defined as platelet count ≥30 109/L and at least 2-fold increase from baseline. Duration of response was defined as time from achieving CR or R to relapse, defined as platelet counts < 30 109/L or bleeding. Patients unresponsive to dexamethasone and those starting second line treatment during the first 3 months were deemed steroid refractory. Data for second line treatment were also collected; type of treatment and response.
Results
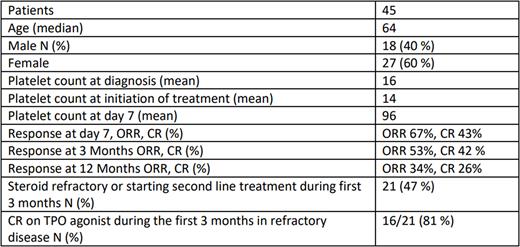
A total of 45 patients were included. Median age was 64 years. In 7/45 patients the dose was reduced to 20 mg. Median number of cycles was 2 (1 - 7). Sixteen patients (37 %) received only 1 cycle of HD-DXM. For most patients (64 %) interval between cycles was 14 days. Patients with active bleeding 20/45 (44%) received additional IVIG. The total dose of IVIG was not recorded. Median observation time for the whole population was 20 months.
The overall response at 3 and 12 months was 53 % and 34%. The low response at 12 months is calculated for the whole population and is presumably falsely low, because 7 patients in CR at 3 months had a shorter follow up with still missing values at 12 months. There was no statistical difference in response at 3 months for patients receiving additional IVIG vs dexamethasone alone or for the number of cycles of dexamethasone. Twenty-one (47%) patients did not achieve a response or started second line treatment during the first 3 months and were considered steroid refractory. As second line treatment patients received eltrombopag (10), romiplostim (6) or other treatments (4), one patient was not treated further. Steroid refractory patients receiving a TPO agonist during the first 3 months achieved a CR in 81 % within a month of starting a treatment.
Of the 24 patients achieving a CR or R at 3 months only 4 (18%) relapsed after a median of 165 days. All four received second line treatment with eltrombopag and all achieved a CR.
Discussion
HD DXM is known to trigger early platelet rise. In our study we found that many patients were treated with only one cycle of HD DXM and those not responding properly, rapidly switched to TPO-RAs during the first 3 months from diagnosis, mostly due to COVID pandemic and trying to avoid longer steroid treatment. To that we can probably attribute relatively low ORR to HD DXM at 3 months (53%), since it is known that repeated cycles up to 4 lead to higher long-term response rates. On the other hand our results suggest early use of TPO RAs could be beneficial for patients refractory to corticosteroids and should not be delayed as 81% of patients that received a TPO-RAs as a second line treatment during the first 3 months achieved a CR. For those responding to HD DXM our results suggest that we can expect durable responses with low relapse rates. Unfortunately, in many countries TPO RAs are not available for treatment of newly diagnosed and persistent ITP. Further data from studies of early use of TPO RAs from real world practice are needed.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal